The Hidden Struggles of Obsessive Compulsive Personality Disorder: When Perfect Isn’t Good Enough
Have you ever had that one friend, family member or just someone you know who has a spotless room, schedules every minute and feels anxious when things just “don’t go right”? Well, I’m certain you know at least one person like that. It could certainly just mean that they’ve mastered the difficult skills of time management and organization and that they just want to be “perfect” and these are really good things but for some people, this can become overwhelming, to a point it becomes damaging. Let’s take a closer look at how that would work.
This can be defined as Obsessive Compulsive Personality Disorder (OCPD). While OCPD is commonly mistaken with obsessive compulsive disorder (OCD) they aren’t the same. Obsessive Compulsive Personality Disorder can be defined as a mental health condition characterized by an excessive need for orderliness, perfectionism, and control, often at the expense of flexibility and efficiency. Due to the extreme need for orderliness, perfectionism and control, OPD can be damaging to an individual’s mental/emotional wellbeing and can sometimes even take a physical toll on one’s body.
Obsessive-Compulsive Personality Disorder (OCPD) and obsessive-compulsive disorder (OCD) sound similar, but they are actually very different in terms of symptoms, causes, and how they affect a person’s life. Here's a clear comparison to help you understand:
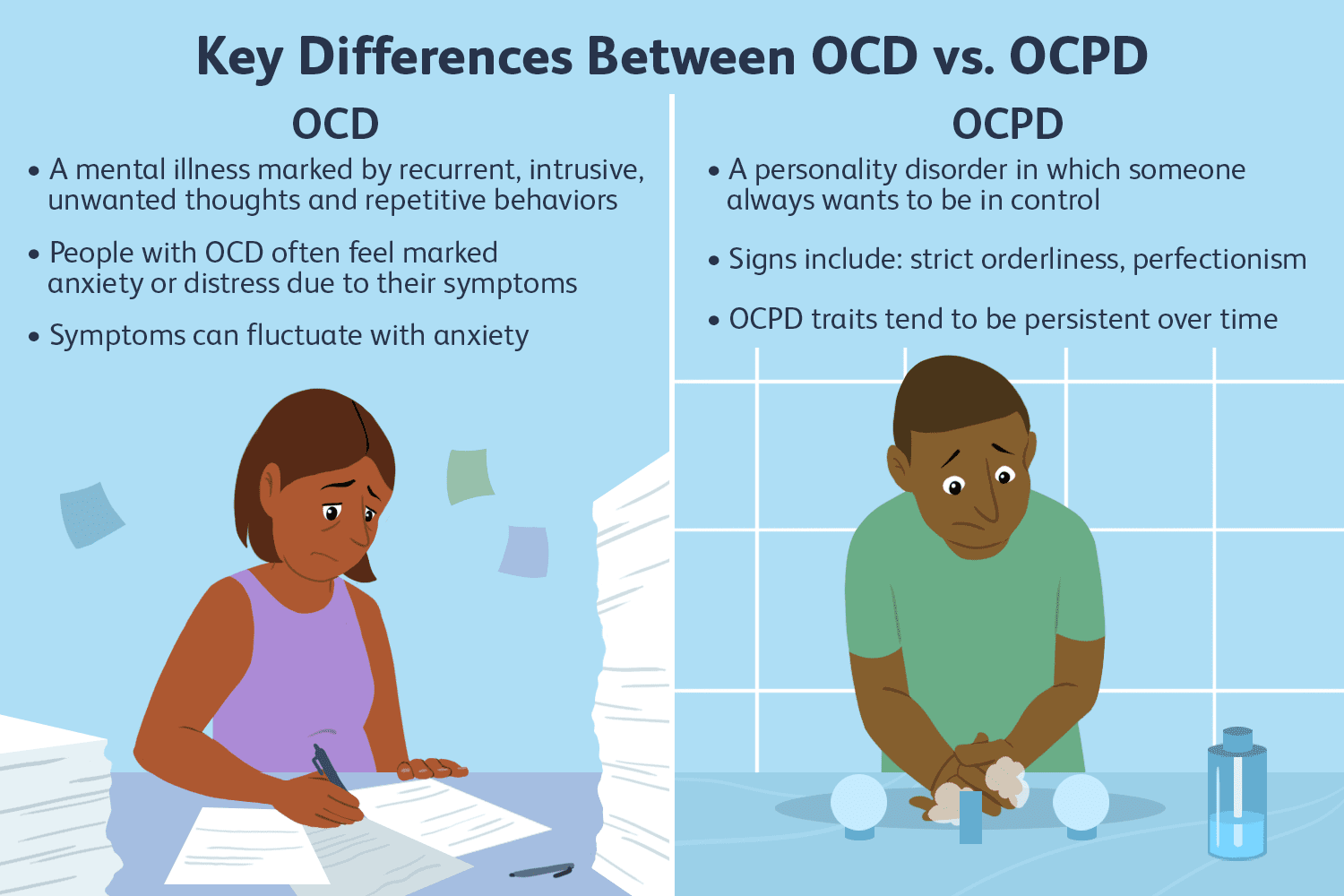
Now that we have understood the difference between OCPD and OCD, let’s look at a few symptoms to identify it.
- Excessive doubt and indecisiveness
- Being unwilling to compromise
- Being unwilling to throw out broken or worthless objects
- Perfectionism that interferes with completing tasks
- Becoming overly fixated on a single task, idea or belief
- Difficulty coping with criticism
The listed above are some common symptoms of OCPD. These symptoms all follow a pattern that doesn’t allow for flexibility and the ability to compromise with others. People with this disorder often don’t realize that their behavior is problematic and affecting those around them.

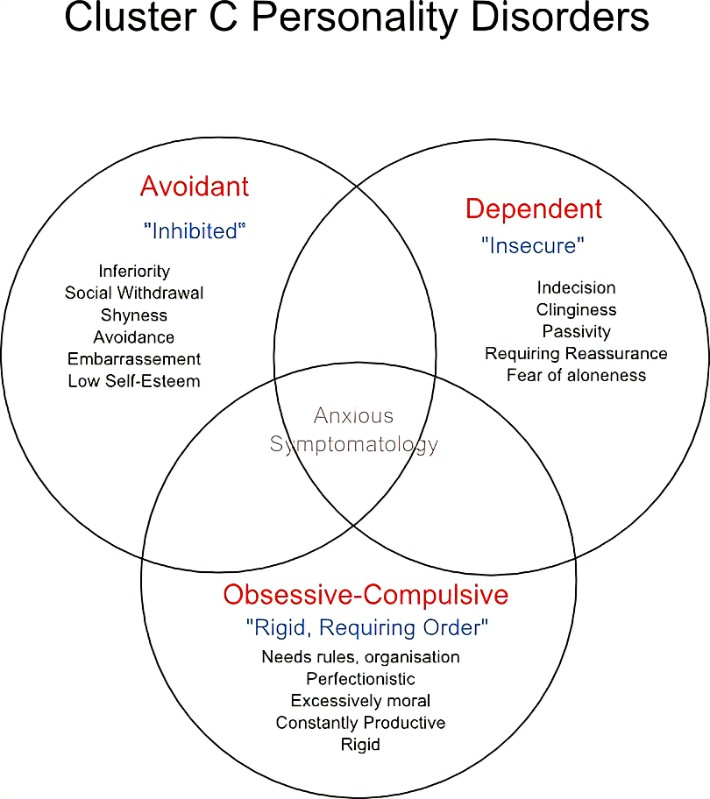
OPCD is one of a group of disorders called the “Cluster C” disorders personality disorders which involve intense emotions of anxiety or fear. Cluster C personality disorders often include avoidant personality disorders, dependent personality disorders and OCPD.
OCPD is considered one of the most common personality disorders. It usually begins in individuals who are in their late teens or early 20s and is most common in adults whose highest level of education is a high school graduation or less. OCPD is most likely to affect individuals with these mental health conditions:
- Anxiety disorders (24%), such as panic disorder and generalized anxiety disorder.
- Mood disorders (24%), such as bipolar disorder.
- Mild to moderate substance use disorders (12% to 25%).
Obsessive-Compulsive Personality Disorder (OCPD) often co-occurs with anxiety disorders, mood disorders, and substance use disorders due to overlapping psychological patterns and shared underlying traits.
Anxiety Disorders (24%):
- Individuals with OCPD have a strong need for order, control, and perfection. The constant striving can generate chronic stress, making them more vulnerable to anxiety disorders like panic disorder or GAD.
- OCPD often involves an intense fear of making mistakes, which aligns closely with the worry and fear that characterizes anxiety disorders.
- These traits can fuel anticipatory anxiety, especially in uncertain or unpredictable situations as people who suffer from this disorder often require constant control over situations.
Mood Disorders (24%):
- The unrealistic standards and rigidity of OCPD often lead to persistent dissatisfaction, which can evolve into depressive symptoms or even episodes of bipolar depression.
- People with OCPD tend to suppress emotions in favor of control, which can worsen mood regulation over time.
- OCD behavior may strain relationships, contributing to intense social isolation and feelings of worthlessness, which are key features of mood disorders. This can be damaging to an individual’s social skills.
Mild to Moderate Substance Use Disorders (12-25%)
- Individuals with OCPD may turn to substances like alcohol or drugs to relieve the pressure of perfectionism or cope with anxiety and internal tension.
- Their rigid thinking may cause them to harshly judge themselves after substance use, creating a cycle of guilt and continued use to numb those feelings.
- Ironically, despite their controlling tendencies, some with OCPD may use substances to momentarily escape their own rigidity and mental overactivity.
The origins of Obsessive-Compulsive Personality Disorder (OCPD) are believed to stem from a combination of genetic, environmental, and psychological factors. While the exact cause is not fully understood, research suggests that individuals may have a genetic predisposition to developing personality traits such as rigidity, perfectionism, and a strong need for control. Environmental influences during childhood also play a significant role—particularly upbringing in households that are overly controlling, emotionally distant, or excessively focused on rules, discipline, and achievement. Children raised in such environments may learn to equate self-worth with productivity and flawlessness, internalizing the belief that mistakes are unacceptable and emotions must be suppressed. This can lead to the development of rigid thinking patterns and behaviors that become deeply ingrained over time. Additionally, early experiences of insecurity or unpredictability may cause a child to rely on order and control as coping mechanisms, which later evolve into the inflexible and perfectionistic traits characteristic of OCPD. These patterns typically solidify during adolescence or early adulthood and persist without treatment.
Due to the obsessive and repetitive nature of OCPD, it can have a detrimental impact on our daily lives. The excessive need for constant control and perfection can be damaging to the individual but also those around them as well. Due to this, it can be difficult to form meaningful friendships and romantic relationships. OCPD can also affect an individual’s professional and school life as it can interfere with completing tasks before deadlines as perfectionism slows down task management. OCPD also eventually leads to intense anxiety, depression and burnout from not being able to establish meaningful relationships and complete tasks efficiently and to an acceptable level.
Being supportive with someone who struggles with OCPD involves a lot of patience, understanding and clear communication with the individual. It is important to recognize that their excessive requirement for control, perfectionism and orderliness stems from OCPD and not stubbornness. Refrain from attempting to “fix” them or trying to change them. Avoid being harsh and criticizing them for their habits and focus on listening empathetically to their problems, but don’t reinforce their antics. Set healthy boundaries when needed, but do so kindly and consistently. Encouraging them to seek professional help, such as therapy, can also be a positive step, but it should be suggested gently, without pressure. Above all, offer steady support through respect, compassion, and calm, even during challenging moments.
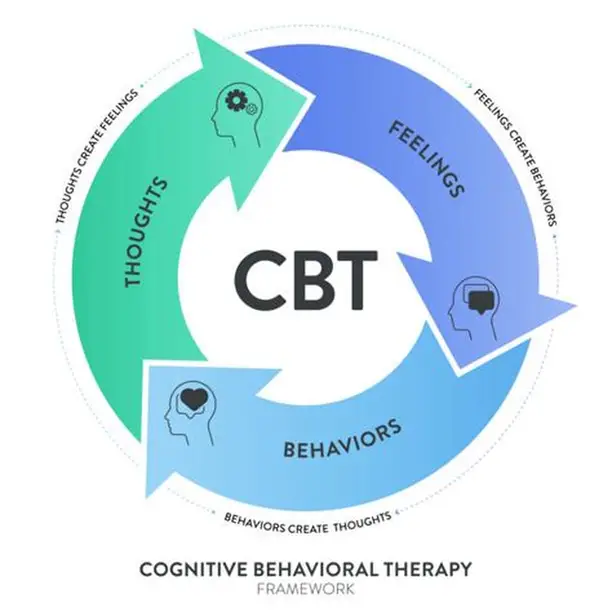
Therapy plays a crucial role in treating Obsessive-Compulsive Personality Disorder (OCPD), as it helps individuals understand the rigid thought patterns and perfectionistic tendencies that interfere with their relationships and daily functioning. Cognitive-behavioral therapy (CBT), in particular, is highly effective in helping patients identify and challenge deeply ingrained beliefs about control, order, and perfection. Through therapy, individuals with OCPD can learn healthier coping strategies, improve emotional flexibility, and develop more balanced perspectives on work, relationships, and self-worth. Over time, therapy can significantly reduce distress and enhance overall quality of life by promoting greater self-awareness and emotional adaptability.
In conclusion, Obsessive-Compulsive Personality Disorder (OCPD) is a complex and often misunderstood mental health condition that significantly impacts an individual’s thoughts, behaviors, and relationships. While it may be mistaken for a strong work ethic or high standards, OCPD goes far beyond simple perfectionism, often leading to chronic stress, interpersonal difficulties, and reduced quality of life. Understanding its origins, symptoms, and effects is crucial for early recognition and effective intervention. With proper treatment—especially through therapy—individuals with OCPD can learn to challenge their rigid thought patterns, embrace flexibility, and build more balanced, fulfilling lives. Increased awareness, empathy, and access to mental health support are essential steps in helping those affected by OCPD find the tools they need to thrive.
Comments ()